In July 2022, Team Med Global surveyed payer enrollment professionals about their job titles, the departments they work in, and those to whom they report. Here’s how they responded:
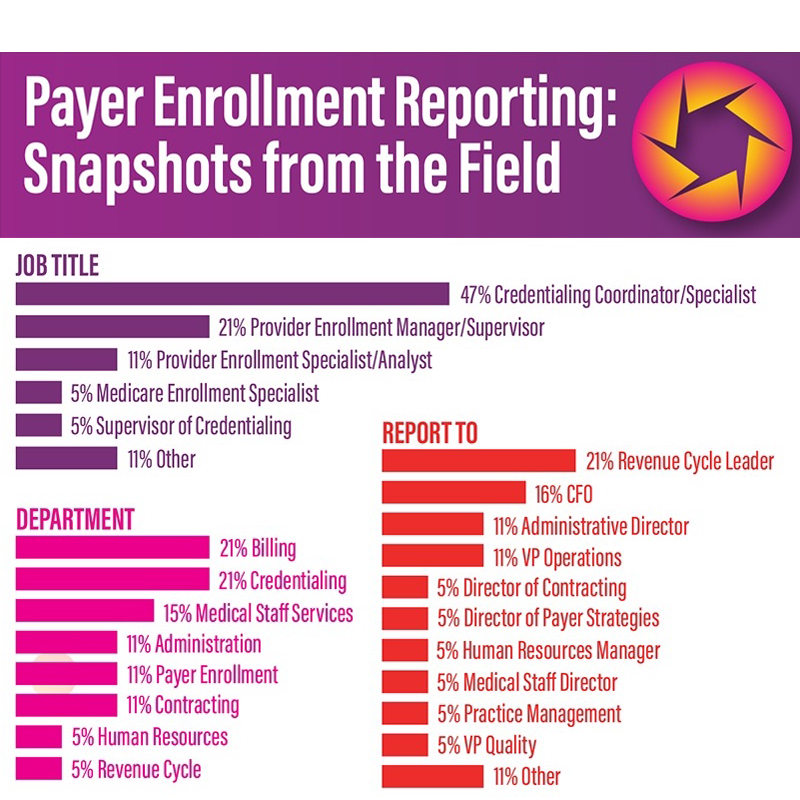
47% Credentialing Coordinator/Specialist
21% Provider Enrollment Manager/Supervisor
11% Provider Enrollment Specialist/Analyst
5% Medicare Enrollment Specialist
5% Supervisor of Credentialing
11% Other
Department
21% Billing
21% Credentialing
15% Medical Staff Services
11% Administration
11% Payer Enrollment
11% Contracting
5% Human Resources
5% Revenue Cycle
Report To
21% Revenue Cycle Leader
16% CFO
11% Administrative Director
11% VP Operations
5% Director of Contracting
5% Director of Payer Strategies
5% Human Resources Manager
5% Medical Staff Director
5% Practice Management
5% VP Quality
11% Other
The data support what payer enrollment professionals have long said, namely that they have a variety of job titles and work environments. This begs the question of whether there are opportunities for standardization within the payer enrollment field.
Ivonne Oladunni, MBA, CPMSM®, is seeing a reversal of the trend to merge credentialing and payer enrollment under a single umbrella. “As organizations and standards continue to grow, employers are segmenting the two,” said Oladunni. “One group of subject matter experts focuses on primary source verification and credentialing, while another group of subject matter experts focuses on the payer side.”

Ivonne Oladunni, MBA, CPMSM®
Oladunni notes that, while the two functions are related, each requires a unique skillset. “Those in credentialing concentrate on the front-end process, investigating and verifying the professional experience of those providing care,” she said. “Payer enrollment professionals move away from the granular information about individual providers and toward a deep understanding of rules and regulations by payers, markets, and states.”
The differences don’t end there. “These are definitely two different segments of the medical staff services world,” said Oladunni. “Many argue that the level of detail needed for credentialing makes it more labor-intensive compared to payers that allow the use of CAQH to submit an application or a delegation roster.” As a result, she says, “The number of files that a credentialing specialist may process at a given time may double in count for a payer enrollment specialist.”
Titles and Reporting
Almost half of those who performed payer enrollment reported having the title of credentialing coordinator or credentialing specialist. Oladunni attributes this to organizations’ placing payer enrollment under the credentialing umbrella. “Organizations may title everyone ‘credentialing specialists’ and then internally differentiate the functions,” she said.
Oladunni says that MSPs and PEPs are challenged with educating leaders and about the difference between credentialing and payer enrollment. “Organizations may not know what they do not know,” she said. Noting that MSPs are still educating leaders on the sequence of the credentialing process, Oladunni sees the need for leaders to understand that payer enrollment picks up where credentialing leaves off. “I’m hopeful that, as we continue to raise awareness through webinars and conferences, shifts in job titles will follow,” she said.
More than a third of respondents indicated that they report to the revenue cycle leader or chief financial officer, which Oladunni says is appropriate. “Payer enrollment rolls up into revenue cycle management and results in bottom line dollars,” she said. “This is the reporting structure I’m seeing most often.” When payer enrollment specialists report to others in an organization, Oladunni says it’s likely because of that organization’s business structure. “Under smaller organizations, for example, individuals may wear multiple hats and have a single, generic title.”
Opportunities to Streamline Payer Enrollment
Oladunni sees a few opportunities to streamline the payer enrollment process. “From the operations side, once a provider accepts an offer from human resources or recruiting, their file should naturally be placed in the credentialing queue for verification and the collection of credentialing documentation,” she said. “At a certain point during that period, if applicable, payer enrollment should aim to have an applicant enrolled prior to their start date. This goal will reduce the need to write off claims on the back end.”
More globally, Oladunni sees potential for automation combined with enhancement of CAQH. “That will allow us to advocate for the use of that repository,” she said. Currently, different payer applications are required based on payer requirements and the state. “If CAQH can be single source of truth for all payers, it will cut down on processing time, and reduce the redundancy of information on applications.”