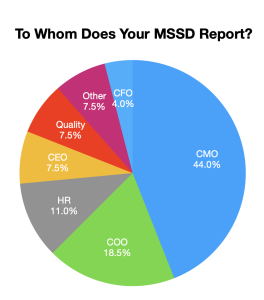
 Team Med Global surveyed MSPs, asking to whom their Medical Staff Services Department (MSSD) reported. The results mirror my experience in the field.
Team Med Global surveyed MSPs, asking to whom their Medical Staff Services Department (MSSD) reported. The results mirror my experience in the field.
Just as standardized processes – from EHRs to telemedicine – have infused the clinical side of healthcare, standardization in MSSD reporting would help the MSP. With a standardized organizational structure, expectations would be better aligned and challenges would be more easily addressed.
Snapshots of MSSD Reporting Structures
Chief Medical Officer (44%): Most frequently, the MSSD reports to the CMO. This relationship dates back to the inception of CMOs, when the administrator’s secretary or assistant would be responsible for credentialing and privileging.
When an organization’s CMO understands the organized medical staff and utilizes their expertise, the CMO becomes the MSP’s go-to person. The CMO’s experience as a practicing physician allows them to quickly answer questions that arise. Because the CMO has their finger on the pulse of what’s happening clinically, they can provide context to issues that arise.
For example, if a doctor is not responding to ER calls within the timeframe established in the bylaws, the MSP can consult with the CMO. The CMO can quickly advise that the physician in question be called to inquire as to their non-response or determine if it’s a habitual problem. In consultation with the department chief, they can refer the matter to the Medical Staff Peer Review Committee.
Reporting to the CMO can be less than ideal when the organization doesn’t have a strong CMO or when the CMO doesn’t have a strong relationship with the medical staff or the C-suite. When that’s the case, the CMO may not have decision-making authority – or not exercise that authority – and the MSP can feel as though they’re swimming against the tide.
Chief Operating Officer (18.5%): COOs understand systems. They see both the big picture of an organization’s strategy and the minute details of vendors, technologies, contracts, and systemization of functions.
Even though the COO may not be familiar with the intricacies of an MSP’s responsibilities, a great COO can grasp the problem the MSP presents and quickly apply lessons learned from other departments. Because they know people across the organization, the COO is a connector who recognizes the value of collaboration and can make the introductions that enable the MSP to get answers.
The COO’s ability to streamline and automate processes can help the MSSD run smoothly. In the process, they help the MSP think more strategically and understand how to build productive teams.
Human Resources (11%): This arrangement works fine for some cultures, but the MSSD isn’t always a natural fit for Human Resources. Many functions between these two departments are similar, such as processing applications, conducting reappraisals, and collecting current licensures. These similar functions seem like the MSSD and HR are a natural fit because of the increase of employed physicians. However, in consultation with legal counsel, great care must be taken to ensure that the confidentiality between medical staff and employment matters remains intact. The MSP must remain diligent in respecting these boundaries.
Chief Executive Officer (7.5%): The CMO and CEO are my favorite reporting structures. With the CEO, you cut out the middleman. If the MSP has an established relationship with the CEO, the MSP can express a concern, state their need, and get an immediate decision.
CEOs and CMOs tend to respect the positions of MSSD leaders and often invite them to administration leadership meetings, board retreats, golf outings, and hospital leadership social events. Administrators see the MSP as a natural extension in building and strengthening relationships with physicians. This elevates the level of respect for the MSSD’s role and the perception of power that MSPs have in an organization.
Quality (7.5%): In the 1980s, when the use of quality data became the focus of administrators, those who worked in Quality didn’t know how to harness their newfound power. As a result, there was a perception by Quality that credentialing and Medical Staff Services should report to them.
While mutual respect between quality and credentialing is warranted, ideally the Quality Department is responsible for managing hospital quality data and information, and complying with regulatory requirements to ensure patient safety. The MSSD is responsible for managing credentialing, privileging, medical staff governance, and physician performance – which includes FPPE, OPPE, behavior, and peer review. The MSSD must work collaboratively with Quality in measuring physician performance. From my years of experience and consultancy, it is my recommendation that the MSSD include one FTE that’s supporting medical staff performance improvement initiatives, including current competence.
Chief Financial Officer (4%): With the growing collaboration between credentialing and payer enrollment, there has been a slight increase in MSSDs reporting to the CFO.
CFOs are typically detail-oriented. This trait aligns with the competencies of MSPs. A CFO is often the administrative leader that oversees the revenue management cycle.
3 Keys to MSP Success in MSSD Reporting
Regardless of the department to which your MSSD reports, there are three critical skills for an MSP’s success: relationship-building, communication, and data collection.
Relationship-building: MSPs work diligently to connect the needs with the practitioner to those of the administration. Establishing strong relationships allows you to serve as each side’s advocate.
In this same realm, be mindful of your personal brand. You want to be known as someone who can navigate and diffuse difficult situations, hold delicate information in confidence, and admit fault when you make a mistake.
Communication: It’s important to understand the administrator’s preferred communication style. If they can’t stand texting, then don’t text them. If they are only interested in the bottom line, don’t write a dissertation. Instead, stick with bullet points.
Similarly, insist on a seat at the table where decisions are made, and then demonstrate your competence when speaking. Articulate your department’s goals and how you propose to achieve those goals.
Data collection: Healthcare is data driven. The time when you can make a request just because you know it to be right is no longer acceptable. Every request made must include the rationale, the benefits, the barriers, and the cost associated with the request, which will allow the administrator to make a data-driven decision.
CMOs, COOs, HR, CEOs, and CFOs are an alphabet soup of MSSD reporting. Our mission as MSPs is to demonstrate our value and maximize our relationships with our administrators, physician leaders, and other stakeholders.